When Hormones Rebel
Understanding, contextualising and recognizing the impact of PCOD/PCOS on Teen Girls
“Your body is a reflection of your life’s story, not just your diet or exercise routine.”
Polycystic Ovary Disorder (PCOD) and Polycystic Ovary Syndrome (PCOS) are increasingly becoming a part of the conversation for women around the globe, especially for young women, teenagers, and working professionals. These conditions, often diagnosed in women of reproductive age, come with a wide range of symptoms that can affect both physical and emotional health. But there’s more to PCOD and PCOS than just a clinical diagnosis — it’s about understanding how deeply these conditions can impact a woman’s life.
When you search online for the difference between PCOD and PCOS, it’s often simplified into a distinction of severity: PCOD is a milder condition, while PCOS is considered a more severe form. However, this explanation fails to capture the real complexity of these conditions. The differences between PCOD and PCOS are not just about severity but also about how the symptoms manifest in each individual. For example, while PCOD typically involves ovarian cysts that result in hormonal imbalance, PCOS may go beyond that, affecting fertility, causing weight gain, and leading to excess hair growth. However, many women with PCOS might never face infertility or excessive weight gain, and not every woman with PCOD will experience cysts. Therefore, the simple idea of PCOD as the milder version and PCOS as the more severe version doesn’t do justice to the complexity of each condition.
Statistically, both PCOD and PCOS are widespread, affecting millions of women worldwide. Globally, it is estimated that between 6-13% of women of reproductive age are diagnosed with PCOD, and the numbers are steadily growing, with many cases going undiagnosed. In India, the prevalence of PCOD is especially alarming — 16% of women in their 20s and 30s are affected, and up to 22.5% of adolescent girls in certain regions are diagnosed with PCOS. These figures speak to the urgent need for greater awareness and understanding. Last year, out of the many adolescent girls I counselled at school, two were diagnosed with PCOD. Their experiences reflect a reality that is shared by many young women around the world. It’s important to recognize that these diagnoses are far more than just statistics — they’re part of real, lived experiences.
For many women, PCOD and PCOS are not just medical conditions — they are deeply emotional experiences. The physical symptoms — irregular periods, weight gain, excessive facial hair, and hair thinning — can be distressing. But often, the emotional pain is far more profound. When a young girl experiences facial hair growth or thinning hair on the scalp, it’s not just a cosmetic issue. It can have a devastating emotional impact, affecting self-esteem and confidence. This is something that cannot be understated. The emotional toll of PCOS/PCOD often goes unnoticed, but it is just as significant as the physical symptoms.
Here’s where the conversation needs to shift. When doctors and gynaecologists diagnose PCOD or PCOS, they often focus on diet, exercise, and weight management as the primary solutions. While this approach is helpful for some, it fails to recognize the individuality of the condition. Not every woman diagnosed with PCOS or PCOD has weight gain or irregular periods. Some women may not experience hair thinning, and others may go on to conceive without medical intervention. The issue is far more nuanced than simply adjusting diet or exercise routines. This is why a detailed case history — which includes understanding the person’s lifestyle, stressors, and emotional health — is critical in forming an effective treatment plan.
In today’s world, where chronic stress has become the norm, many people fail to recognize the toll it takes on the body. Stress, both physical and emotional, has a profound impact on our hormonal health. When stress levels are high, the body releases cortisol, a hormone that triggers the body’s fight-or-flight response. While this response is meant to be short-term, chronic stress keeps the body in this heightened state, wreaking havoc on hormones like insulin and androgens. These imbalances can exacerbate or even trigger PCOD and PCOS symptoms. The link between chronic stress and hormonal imbalance is undeniable. And the truth is, many women living with PCOS and PCOD often have backgrounds of trauma or stress that make simple lifestyle changes like diet or exercise incredibly difficult. The exhaustion, both mental and physical, caused by ongoing stress can make even basic daily activities feel overwhelming. When the stress response is prolonged, it can lead to hormonal dysregulation that directly contributes to the worsening of PCOD/PCOS symptoms.
In my experience as a counsellor, I’ve seen how stress not only affects a person’s ability to function day-to-day, but how it impacts their ability to heal. One of the two young girls I counselled, both diagnosed with PCOD, had a backdrop of chronic stress. The pressures of school, relationships, and future uncertainty had left her feeling physically exhausted and mentally drained. For many women, this constant state of stress becomes a barrier to getting better. It’s not just about weight management or exercise; it’s about managing the emotional and psychological burden that comes with living in a world that demands so much. Healing, therefore, needs to be holistic — it’s not just about addressing the physical symptoms but also addressing the emotional roots that contribute to the condition.
Furthermore, PCOS and PCOD are often seen through the lens of biomedical treatment — medications like hormonal birth control, anti-androgens, and fertility drugs are commonly prescribed. While these treatments may help manage symptoms for some, they do not always offer long-term solutions. The biomedical model, in its current form, tends to focus on symptom management rather than exploring the root causes, and this often leads to frustration among women who feel their health concerns are being reduced to a prescription list.
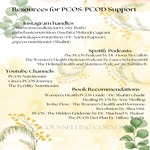
But there is hope. More women are starting to embrace a holistic approach to healing — one that considers lifestyle changes, emotional well-being, and natural remedies. Influencers like Suchita Mukerji Gagrani, who turned her own PCOS diagnosis into a path toward creating wellness products like her PCOS Herbal Tea, have shown that healing can come from more than just pills. These alternatives offer hope for many women who want to take control of their health in ways that feel more in tune with their bodies. Cory Ruth, a nutritionist who specializes in diet for women with PCOS, has shown how food can become medicine — offering a way to balance hormones through diet, without resorting to harsh treatments or extreme lifestyle changes. These stories highlight the growing movement of women who are using their own experiences to find alternatives to traditional biomedical treatments.
However, it’s also important to acknowledge the rise of a wellness market that promises quick fixes — from rosemary oils for hair loss to hormone-balancing teas. While rosemary has been shown to be as effective as minoxidil for promoting hair growth, it’s important to approach these products with caution. The effectiveness of rosemary in treating hair loss is well-documented, but with its rise in popularity, many companies are jumping on the bandwagon, selling fake or low-quality versions that are not nearly as effective. This exploitation of a natural remedy undermines the potential benefits it could offer to those seeking alternative treatments for hair thinning and hormonal imbalances. While rosemary may offer relief for some, it’s important to ensure that any products you use come from reputable sources, and should never replace professional advice or personalized care.
In the end, PCOS and PCOD aren’t just medical conditions; they are signposts of the times we live in. They reflect the toll that chronic stress, societal expectations, and emotional burdens take on women’s bodies. And as we move forward, it’s crucial that we reframe the conversation around these conditions. It’s not just about managing the symptoms — it’s about understanding that healing comes when we embrace the full picture: the physical, emotional, and psychological health of the individual. Parents, educators, and healthcare professionals need to work together to ensure that women diagnosed with PCOS and PCOD feel supported, heard, and empowered to take control of their health in a way that suits their unique needs.
* If you or someone that you know is struggling with PCOD/PCOS